It’s Spring Semester of our second year of PT School!!!!
I feel like this semester things are starting to really come together, in terms of my study habits and just in general feeling like I have a grasp on things. We’re back up to a full schedule: 3 classes with 2 labs…..plus this semester we started our research project!
Our professors are now trying to prepare us for our upcoming acute and neuro internships, which in my program will be this fall and next spring. So this semester we are taking Neuro II and Cardiopulm, which both have labs, and a class called Advanced Movement which is basically Biomechanics II.
I find these classes very interesting and helpful in preparing us for our upcoming internships (although nothing really truly prepares you lol <cry cry> lol)
So here is a list of some of the things I have learned in this first month of my 5th (:o) semester of PT school:
Cardiopulm
- General understanding of cardiopulm prevention strategies: diet, exercise, sleep, etc.
- Different kinds of triglycerides, levels of cholesterol that are appropriate for best health, dietary recommendations for things like sodium, cholesterol, calories, etc.
- DASH diet
- In-detail heart anatomy
- ECG strips and how to read them
- Nitric Oxide is a vaso-dilator
- Atrial kick is the final 1/3 of blood that flows into the ventricles when the atria squeeze (the first 2/3rds flow into the ventricles passively)
- Starling’s Length-Tension Relationship
- Cardiac Output CO = HR x SV
- Normal ejection fraction is 55%-75%
- The visceral pleura is not pain sensitive, and the parietal pleura is pain sensitive. This means that diseases affecting the lungs can be pretty advanced before they’re discovered.
- The body regulates breathing and pH levels through CO2 chemoreceptors. For patients with COPD and other obstructive diseases, their bodies become somewhat accustomed to higher CO2 levels, so they rely on O2 levels. So we would not want to titrate their O2 to a high level because they would stop breathing! Above 90% pulse ox is fine for these patients.
- Decreasing BP and increasing HR = a medical emergency
- We also talked a lot about what constitutes emergent vs urgent situations.
Cardiopulm Lab
- Relaxation Techniques – ahhh what a great day this was! I love in PT school when we get to try out the therapies on ourselves, especially lovely things like massage and relaxation techniques. This day in lab was full of slow breathing and guided imagery. It was truly a great, great day.
- Coronary arteries receive their blood flow during diastole (if you already didn’t know)
- Heart is innervated by sympathetic and parasympathetic nervous systems
- Norepinephrine increases the heart rate (chronotropy) and force of contraction (inotropy)
- Epinephrine is stimulated by the sympathetic NS and is part of normal exercise response
- The parasympathetic NS influences the heart by the vagus nerve. The heart is also influenced by baroreceptors and chemoreceptors.
- Reviewed Predicted Max HR, Karvonen Formula, VO2R, METs, Talk Test, RPE, Berg Perceived SOB scale
- Light exercise is 30-39% of HRR, Moderate 40-59%, Vigorous 60-89%

We also did an exercise response lab where we went to the gym with a group. We had one person exercise on the bike for 10 minutes, plus 5 minutes of warmup and 5 minutes of cooldown. We took her HR, BP, RR, and RPE at the following points:
- At rest
- 5 minutes of warm-up
- 5 minutes into the higher intensity biking
- 10 minutes into the higher intensity biking
- After 5 minutes of cooldown
This seems like a pretty basic activity, but it was really nice to actually get the chance to do it, and drill it into ourselves what we are supposed to do and how frequently.
Another day in lab was spent learning how to find measure body composition using skinfold calipers. I didn’t find this process to be super scientific. So we also discussed more recent body composition technologies like the BOD POD (lol), Hydrostatic Weighing, Dual-Energy X-Ray Absorptiometry, Electrical Impedance, waist circumference (old-school) and of course the famous BMI which is kg/m^2 🙂
And we also learned how to put on abdominal binders and TED hose which help to prevent DVTs.
Neuro
Neuro this semester became quite fascinating. Previously we had focused on neurological anatomy and function – the various tracts of the spinal cord, the functions of different parts of the brain, how nerves transmit impulses, etc.
This semester was focused on neurological pathologies and PT treatment so….yay!
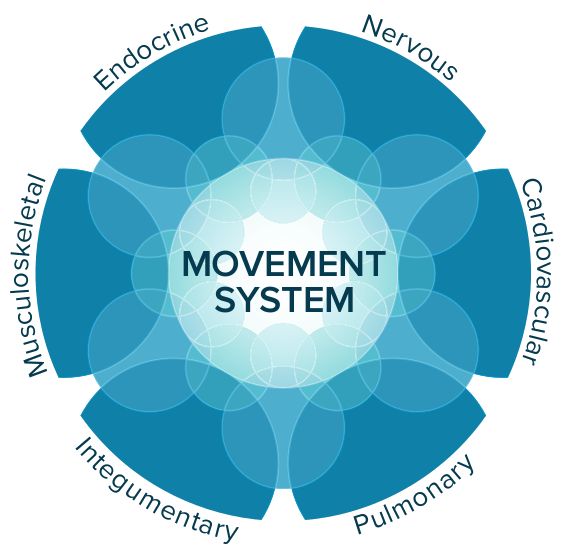
- We started by talking about viewing the patient in terms of their whole movement system and how we as PTs are the experts in the movement system. This is a new focus the profession is leaning towards, and it is a good way to help differentiate us from other medical professionals, and emphasize the fact that the whole movement system is our area of expertise. I really love that.
- We also talked about the general functional issues a patient with neurological deficits might encounter, including driving and assistive devices.
- Vestibular issues! We discussed the many types of vestibular issues a patient might have including vertigo, dysequilibrium, oscillopsia, nystagmus, saccades, and presentation of all of these. We also discussed how to differentiate between central and peripheral lesions for vestibular issues.
- Parkinsons: we delved more into the pathophysiology of this disease, and the physical therapy treatment of it, which is mainly using big, expansive movements and external cuing. There is a lot more to it than that, but that’s the very essence of it.
Neuro Lab
So. much. fun.
Vestibular Tests
- Foam and Dome (see the Insta post above 🙂
- Head Thrust Test (aka Head Impulse test) – you tilt their head down 30 degrees, tell them to focus on your nose, and shake their head back and forth rapidly, then quickly move to L or R and check if their eyes are shaking or have a delay.
- Head Shaking Nystagmus test – Same as above, but their eyes are closed and you stop them as they are looking at your nose and you tell them to find your nose.
- Fukuda Step Test – mark the floor where the patient is standing. Have the patient hold their arms out, close their eyes, and march for 50-100x. When they are done, observe how much they’ve moved.
- Dynamic Visual Acuity Test – a normal test with a Snellen Chart EXCEEEPPPPTTT they are moving their head side to side at a rate of 1 side per second and read the line they can see. This line should only be 1 line higher than the normal line they can read. This tests their Vestibulo-ocular reflex (VOR)
- BPPV tests: Dix Hallpike for anterior and posterior canals; Horizontal Canal test for ummmmmm horizontal canal.
Vestibular Treatment
- Corrective Saccades
- VOR X1 and X2
- Epleys for anterior and posterior canal BPPV
- BBQ Roll for horizontal canal BPPV
PNF
D1 and D2 flexion and extension for UE and LE including rhythmic initiation, repeated contractions, reversal of antagonists, alternating isometrics, rhythmic stabilization, quick stretch, hold-relax, contract-relax
Functional Postures
Basically Table 10.6 in OSullivan aka one of the best books known to humankind!!!!
Sensory Stimulation Techniques
Basically Table 10.9 in OSullivan, did I mention one of the best books known to humankind!!!!
Parkinson’s Treatment
We talked about evaluating a patient with Parkinson’s including their prior level of function (PLOF), assistive devices, and home environment. And of course the more physical type of therapy, where we emphasize big movements and use auditory stimulation like music or a metronome to help patients move.
Advanced Movement
I consider this class basically Biomechanics II. We added onto our previous study of the biomechanics of gait. We analyzed each part of the TUG test:
- Sit to Stand
- Gait initiation
- Turning
We also studied the TUG test itself and its reliability plus Tinetti. We then analyzed the gait cycle of stair ascent and descent including all of its different phases. Then we did the same with running.
We also spent some of our lecture time in the Biometrics lab using things like handheld dynamometers, grip dynamometers, Biodex, the shuttle, forceplates, sensors, balance foot plates, the Neurocom….I LOVED this. It was so great to use all of this equipment in our hands and try it all out both as the therapist and the subject. I love on the hands-on-ness of PT!!